About Us
"As researchers, it's our duty to expand the scientific knowledge of MS. I truly believe it is possible to find a cure for this disease"
- Dr. Saud A. Sadiq
Multiple sclerosis (MS) is a chronic disease of the central nervous system that affects the brain, optic nerves, and spinal cord. MS is also an autoimmune disorder, meaning that the patient's own immune system attacks their nerve tissue.
MS is characterized by the destruction of the myelin sheath, a layer of insulation that surrounds nerve cells and serves the dual purpose of strengthening nerve signals and protecting the fibers that connect nerve cells to each other. As myelin breaks down, lesions appear and form hard plaques, or sclerosis, which give the disease its name. MS may affect more than 2.5 million individuals worldwide, but there is no full understanding of the cause and mechanism of the disease.
Tisch MSRCNY is at the forefront of advances in the field of neuroimmunology and is determined to discover the cause of, and the cure for, MS.
History of Tisch MSRCNY
Dr. Sadiq began directing a 320 square foot laboratory at the Columbia University Medical Center, and dedicated his career to finding the cause and cure for multiple sclerosis.
In 1998, Dr. Sadiq moved to the Department of Neurology at St. Luke's-Roosevelt Hospital and reformed the center as the MS Research and Treatment Center, upgrading to a 2000 square foot facility. With increased funding, the research wing more than doubled in size in 2003 and expanded to 10 researchers.
In 2006, Dr. Sadiq left the hospital/university setting and opened the Multiple Sclerosis Research Center of New York (MSRCNY), an independent, private, not-for-profit 501(c)(3) research institute. Then and now, it is the largest independent MS center in the world.
With the generous assistance of our benefactors, we initiated a further expansion. The current facilities are approximately 80,000 square feet, and house the latest in research equipment and technology designed to accelerate the pace of MS research and treatment. The expansion included the installation onsite of two 3-Tesla magnetic resonance scanners to serve our clinical and research needs.
In recognition of the Center's achievements in MS research, the Tisch family named the research center in February 2013. Tisch MSRCNY is a nonprofit organization supported entirely by grants and private philanthropy. The close relationship of the research center and the clinical practice, International Multiple Sclerosis Management Practice (IMSMP), speeds the translation of science into clinical practice and helps to test new treatments for MS. Combined, the two entities have a staff of 80+ individuals dedicated to accelerating the pace of scientific discovery and advancement at minimum cost and with minimal bureaucratic constraints.
Our Values
Scientific Rigor
We are committed to the highest level of scientific precision and accuracy, ensuring our findings are robust, reliable, and contribute meaningfully to the understanding of multiple sclerosis.
Transparency & Integrity
We uphold the highest ethical standards and ensure transparency in all our research, communications, and collaborations, building trust with the MS community.
Mentorship
We believe in fostering the next generation of researchers and clinicians through dedicated mentorship, promoting growth, and knowledge sharing.
Principal Investigators
Bringing together the brightest minds in MS.
Details

Saud A. Sadiq, MD, FAAN, is the Chief Research Scientist and Director of the Tisch Multiple Sclerosis Research Center of New York (Tisch MSRCNY) and Founder and Director of the International Multiple Sclerosis Management Practice. These two institutions opened their doors together in 2006 and constitute the largest independent facility dedicated to MS in the world.
A neurologist, neuroscientist, and internationally recognized leader in multiple sclerosis research and patient care, Dr. Sadiq has dedicated more than three decades to advancing understanding of MS and developing novel therapeutic approaches. Under his leadership, Tisch MSRCNY has grown into one of the world’s premier MS research institutes, known for its bench-to-bedside innovations and groundbreaking work in regenerative medicine.
Dr. Sadiq trained in internal medicine and neurology in Kenya, the United Kingdom, and the United States before completing a research fellowship in neuroimmunology at Columbia University. His academic career includes faculty appointments at Columbia University, Albert Einstein College of Medicine, and St. Luke’s–Roosevelt Hospital Center, where he served as Chairman of Neurology and Rehabilitation Medicine. Over the years, he has directed numerous MS research programs, chaired clinical and academic committees, and mentored dozens of research and clinical trainees who now hold positions across the globe.
An accomplished investigator, Dr. Sadiq’s research focuses on the molecular mechanisms of MS, the triggers of autoimmune activation, biomarkers of disease activity, and—most notably—repair and regeneration within the central nervous system. He has led Phase I/II clinical trials, pioneered intrathecal treatment approaches, and secured extensive foundation and philanthropic support for the Center’s stem cell and regenerative neurology programs. He is credited in over 100 scientific publications and has mentored over 140 young scientists through the Tisch MSRCNY Research Assistant Program.
Dr. Sadiq is a Fellow of the American Academy of Neurology and a member of the American Association for the Advancement of Science, the Society for Neuroscience, and the International Society for Stem Cell Research. He has been recognized repeatedly as one of New York’s top neurologists, earning honors from New York Magazine, Castle Connolly, and numerous patient-driven awards. He has delivered lectures at major academic institutions and global scientific forums, and served as a reviewer for over 2 dozen scientific journals.
Through his dual commitment to cutting-edge research and compassionate patient care, Dr. Sadiq continues to shape the future of multiple sclerosis treatment. His work at Tisch MSRCNY and IMSMP reflects a central mission: to uncover the mechanisms of MS, drive innovation in therapeutic development, and improve the lives of people living with MS worldwide.
Details
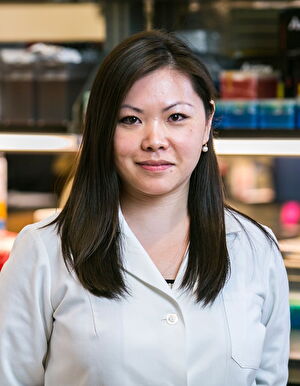
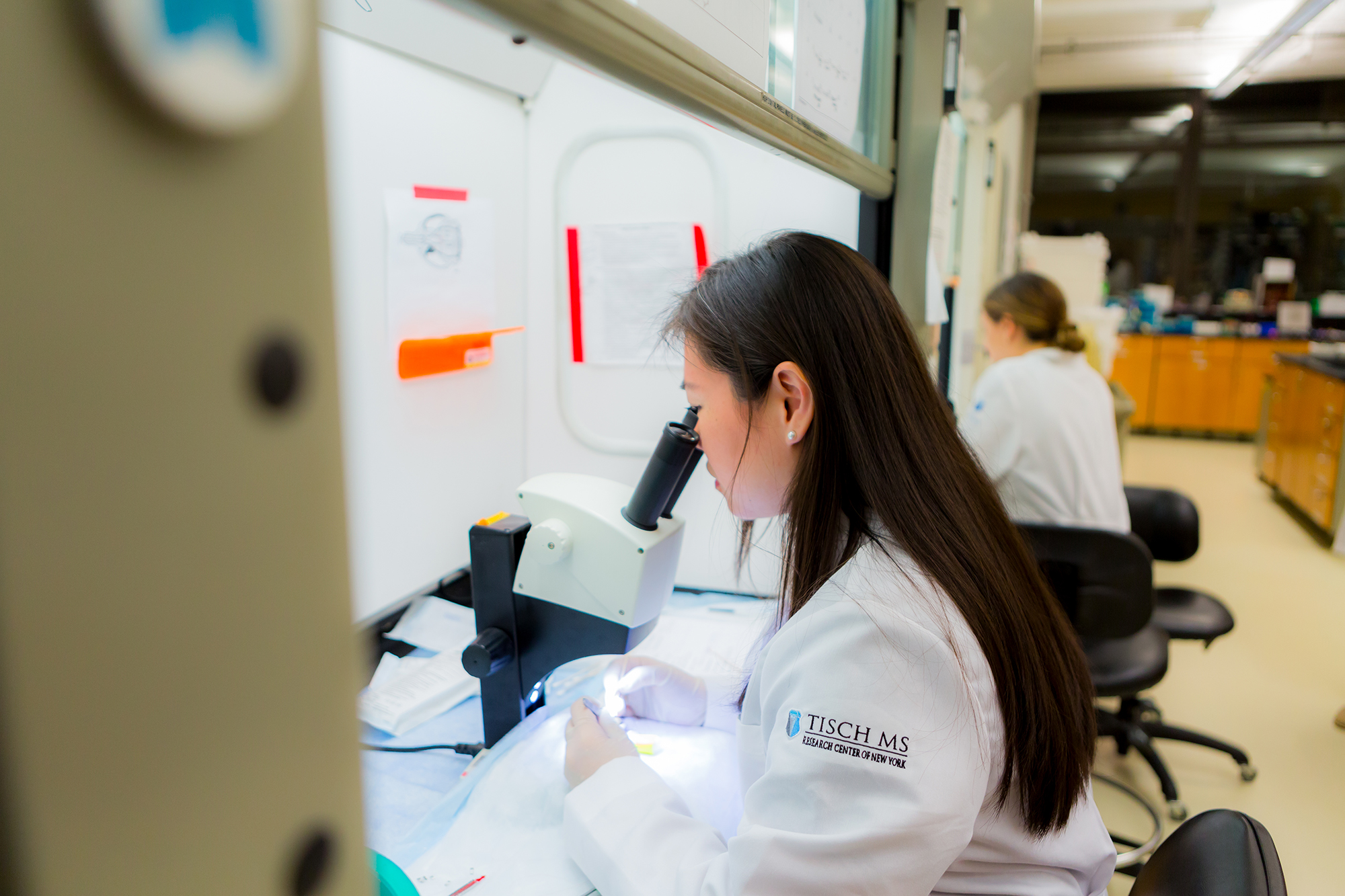
Dr. Harris joined the laboratory of the Tisch Multiple Sclerosis Research Center of New York in 2004, where she has been developing cell therapy strategies to promote repair and regeneration in multiple sclerosis. Her work has led to the groundbreaking stem cell clinical trial, the first ever to test bone marrow-derived neural progenitors in patients with MS. Through investigating adult stem cells from bone marrow- a source of cells from the same individual (autologous) - known as mesenchymal stem cell-derived neural progenitors (MSC-NPs), Dr. Harris, and her team have discovered that these cells promote repair in areas of demyelination when injected into mouse models of multiple sclerosis. Compared to MSCs, MSC-NPs are enriched in signaling molecules that are implicated in their therapeutic effects in MS.
Through the uniquely close partnership between the researchers, clinicians, and patients, this stem cell therapy was tested in twenty MS patients through an FDA approved Phase I clinical trial. Results from the study were remarkable and unprecedented. Patients with both primary and secondary progressive MS experienced improvement in bladder function, vision, and walking speed with no adverse effects. Long term followup of the Phase I patients suggested that some of the neurological improvements were sustained.
A placebo-controlled, double-blind Phase II study was recently completed and demonstrated significant improvements in walking speed and endurance after MSC-NP treatment, providing additional evidence of the neurological benefits of this novel cell therapy. Dr. Harris oversees the Tisch MS Regenerative Medicine Laboratory and the manufacturing of clinical-grade doses of autologous MSC-NPs for cell therapy treatments in trial subjects with MS. Dr. Harris and her team are actively investigating the mechanisms by which MSC-NPs promote repair and regeneration in MS. MSC-NPs promote repair through a bystander mechanism, where they release a number of molecules that impact damaged cells in the brain as well as activated immune cells. Biomarker analysis in MS patients receiving MSC-NP treatment showed that biomarkers associated with activated microglia are altered in response to the treatment. Microglia are resident immune cells in the brain and their chronic activation is associated with MS disease progression. Utilizing iPSC-derived microglia, Dr. Harris has shown that pro-inflammatory microglial activation is attenuated in the presence of molecules released by MSC-NPs. Identification of the molecules involved in MSC-NP-mediated repair will have therapeutic potential in future cell therapy strategies.
As regenerative therapies are developed and tested in clinical trials, there is a need for biomarkers that can measure neural repair and remyelination in MS. Cerebrospinal fluid (CSF) circulates around the brain and spinal cord and, thus, is ideally suited to measure neural repair. Dr. Harris’ research team is investigating the CSF of patients treated with stem cells or other MS medications in order to discover novel disease biomarkers. In a review article, Dr. Harris and Dr. Sadiq discuss the benefit of using CSF biomarkers as a means to understanding the level of disease activity and treatment response in MS patients. For example, newly discovered CSF biomarkers that change following MSC-NP treatment will help identify patient subpopulations that are most likely to respond to treatment. Through her expertise in studying biomarkers, Dr. Harris and her team are revealing a better understanding of disease mechanisms that lead directly to personalized treatments for patients.
Dr. Harris has had a longstanding interest in stem cell biology and in understanding the mechanisms of cell signaling and differentiation. She received her PhD in Pharmacology from Georgetown University, and her BA in Biochemistry/Molecular, Cellular, and Developmental Biology from the University of Colorado in Boulder. Her training also included a postdoctoral fellowship at Mount Sinai Medical Center in New York, where she studied mechanisms involved in the maintenance of cancer stem cells.
Details
Dr. Wong’s research career has been dedicated to studying pathophysiological mechanisms underlying central nervous system injury (CNS) injury and disorders, with the goal of identifying therapeutic targets to promote CNS regeneration and repair. Dr. Wong received her Ph.D. in Biological Sciences, and B.S. in Neurobiology from the Neurobiology and Behavior Department at University of California, Irvine. Her thesis work focused on evaluating the impact of plasticity-promoting drugs and motor training on locomotor recovery following spinal cord injury. Dr. Wong completed a postdoctoral fellowship at Icahn School of Medicine at Mount Sinai in New York, where she investigated molecular signaling pathways and epigenetic mechanisms which can be manipulated to improve ischemic injury following stroke, and enhance axon regeneration following spinal cord injury.
In 2015, Dr. Wong became a principal investigator at Tisch MSRCNY, where she oversees the Experimental Research Center. She has used her surgical expertise to develop the first animal model for primary progressive MS (PPMS) via intrathecal injection of PPMS patient cerebrospinal fluid (CSF) into the cervical spinal cord subarachnoid space in mice. This PPMS animal model exhibits hallmark MS pathology including: demyelination, reactive astrogliosis and axonal damage, which consistently manifests as forelimb motor deficits. In a landmark publication, Dr. Wong reported that pathogenic antibodies in CSF are a distinctive feature of PPMS. Using her animal model, Dr. Wong and her team discovered that only PPMS CSF or recombinant antibodies (rAbs) derived from B cells in PPMS CSF induced motor disability and hallmark MS pathology in the cervical spinal cord, the region that is predominantly affected in PPMS patients. This was not observed with CSF or rAbs from relapsing-remitting MS (RRMS) or secondary progressive MS (SPMS) patients.
Dr. Wong has also used the same surgical approach to develop a specific animal model for sporadic amyotrophic lateral sclerosis (sALS), a previously unmet need. ALS is a fatal neurodegenerative disease characterized by motor neuron degeneration. In 90% of ALS patients, the disease arises sporadically with unknown cause, while only 10% develop familial ALS (fALS) due to inherited gene mutations. Dr. Wong and her team discovered that CSF from sALS patients, but not fALS patients, induced hallmark ALS pathology including upper and lower motor neuron degeneration and cytoplasmic TDP-43 translocation, resulting in motor disability. Dr. Wong reported the identification of apolipoprotein B-100 (ApoB) as the neurotoxic factor in sALS CSF responsible for inducing motor disability and motor neuron degeneration, using a series of CSF filtration studies and proteomic analysis.
In both PPMS and sALS studies, Dr. Wong and her team have demonstrated that CSF filtration can successfully remove pathogenic or neurotoxic factors from CSF, which subsequently attenuates the pathogenic capacity of CSF to induce clinical symptoms and disease pathology. Dr. Wong is a member of the NeurapheresisTM Research Consortium, which is geared towards advancing the use of CSF filtration therapy in various neurological conditions.
Active ongoing projects in Dr. Wong’s team include: 1) elucidating mechanisms underlying antibody-mediated pathology in PPMS, 2) understanding how elevated ApoB and cholesterol dysregulation leads to motor neuron degeneration in sALS, 3) testing potential therapeutics in animal models of PPMS and sALS, 4) investigating why RRMS patients transition to SPMS, and 5) understanding cerebellar dysfunction in MS.
Details
Dr. Daviaud joined the Tisch MS Research Center of New York in January 2019. His research focuses on understanding the pathological basis of the diverse clinical phenotypic expressions of multiple sclerosis (MS).
Dr. Daviaud’s research was conducted through a first-of-its-kind, non-immune-based human model of MS, that uses patient stem cells to generate “mini-human brains” called cerebral organoids. Cerebral organoids recapitulate early human neurodevelopment, including the generation, proliferation, and differentiation of neural precursor cells into glial cells and neurons and their interactions. This innovative model of MS allowed us to study the patient’s genetic contribution to the onset and development of MS, as well as its interplay with environmental triggers, such as viral infection.
Dr. Daviaud and his team developed cerebral organoids from patients with primary progressive MS (PPMS), secondary progressive MS (SPMS), and relapsing remitting MS (RRMS) as well as from healthy controls. His findings demonstrated that organoids derived from patients with MS can be used as an innovative tool to better understand the genetic basis for the phenotypic differences seen in MS. The finding that a patient's genetic background can directly alter stem cell function provides new insights into innate cellular dysregulation in MS and identifies the p21 pathway as a new potential target for therapeutic strategies in MS.
Dr. Daviaud has a long-standing passion for modeling and studying disease pathophysiology and developing innovative therapeutic approaches. He received his Ph.D in Neuroscience from the University of Angers, France. His thesis work focused on the development and characterization of pharmacologically active microcarriers conveying stem cells for the treatment of Parkinson’s and Huntington’s diseases. As a postdoctoral fellow training at the Icahn School of Medicine at Mount Sinai, he studied the use of cerebral organoids as a new human model of preterm hypoxic injury, as well as the engraftment of transplanted human cerebral organoids in the mouse cortex for neural repair in cases of brain injury or neurodegeneration.
Details
Dr. Alfonso joined the Tisch Multiple Sclerosis Research Center of New York as a Research Associate in January 2020, where he focuses on the study of the association between MS and the strongest environmental risk factor linked to this disease, infection with Epstein-Barr virus (EBV). EBV main cellular target within the host are mature and memory B-cells where it stablishes life long-latency. Infection of epithelial cells through a lytic phase is also fundamental for the normal life cycle of the virus, and additional cellular targets like T-cells and NK cells have been described in the context of pathogenesis. By growing different EBV strains in tissue culture, Dr. Alfonso performs in vitro infection of cells of the central nervous system relevant to MS pathogenesis. Using different infection approaches and cellular models, the aim of the lab is to address the significance of this infection and the mechanisms involved.
Dr. Alfonso is also interested in studying the immunological configuration of untreated and treated MS patients. Most MS therapies with high-efficacy are known to alter the patient’s immune system, including changes in the number of blood cells, their body distribution and/or function. Importantly, a need to understand the impact of high-efficacy disease modifying treatments on the immune response to microbe and vaccination challenges is of vital importance as it became apparent during the COVID-19 pandemic. To better understand the potential immunological limitations to challenges due to immunomodulatory treatments, Dr. Alfonso has examined the immunological configuration of MS patients treated with anti-CD20 who were exposed to COVID-19. In work published in 2022 and 2023, his group presented evidence of a strong T-cell response even with limited antibody-based response suggesting some level of immune protection in this group of patients. In connection to the effort to study EBV’s role in MS disease, Dr. Alfonso’s group wants to also look at the immune response to EBV and its progression during disease and treatment. Understanding the level of dysregulation of the immune system during MS disease and specifically in response to EBV infection could help decipher the pathogenic roots of this neurological disease.
Dr. Alfonso has extensive experience in the study of virus-host interaction at the cellular-molecular level with more recent immersions in the field of immunology. He obtained his Ph.D. at the National Center for Biotechnology in Madrid, Spain, where he studied the role of epigenetic host factors in the replication and pathogenesis of influenza virus. His postdoctoral training at the National Institutes of Health (NIH) in Bethesda, MD, was focused on the regulation of Herpes virus gene expression during lytic and latency phases and the discovery of new host-virus interactions.
Details

Dr. Yan began working in our research laboratory in 2005. After some recent work in China, Dr. Yan rejoined Tisch MSRCNY in 2019 as a Research Scientist. His research focuses on providing pathological expertise to our scientists. Almost all of our investigations involve the use of brain and spinal cord specimens. These tissues are obtained from patients with multiple sclerosis who have generously and selflessly donated their bodies for medical research. Such samples are difficult to obtain and at Tisch MSRCNY, we are fortunate to have well-preserved tissue specimens. Dr. Yan’s work has involved extensive cataloging of various sections of normal and MS affected brain, as well as categorizing MS lesions into "active" and "inactive." In addition, the Center has spinal cord sections from the cervical and thoracic spine at different levels. The availability of these specimens is especially critical to our work. Based on his past experience with pathological specimens, staining, and categorization pathology, Dr. Yan collaborates with other researchers on their projects in finding the cause of MS and to elucidate a better understanding of progressive disease.
Dr. Qijiang Yan received his PhD in Neurobiology from Sun Yat-sen University of Medical Sciences in Guangzhou, China and an MS in Anatomy from China Xinjiang Medical University.
Details
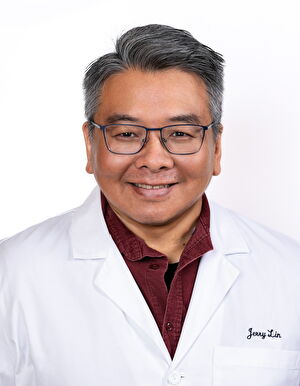
Jerry Lin has collaborated with Dr. Sadiq since 1996, where he worked as a research assistant at Columbia University Presbyterian Hospital under Dr. Sadiq and Dr. Norman Latov. As a research associate, he helped establish Dr. Sadiq’s research program at the MS Research & Treatment Center at Roosevelt Hospital from 1998-2006, and subsequently as a senior staff associate at the MSRCNY (now the Tisch MSRCNY) from 2006 to present. His motivation for continual research lies in his strong work ethic and understanding that Dr. Sadiq cultivates a unique and collaborative environment at the Center. Mr. Lin is a graduate of Johns Hopkins University with a BA in Chemistry.
Lin is actively working towards discovering the cause of MS. His research is based on the finding that over 90% of MS patients have oligoclonal bands- antibodies that identify and aid in the removal of foreign antigens such as viruses and bacteria- in the cerebrospinal fluid (CSF). Lin believes that finding the targets of these antibodies may lead us to the cause of the disease. Lin and his team have developed the techniques to successfully isolate clonally expanded and persistent B-cells from the CSF of MS patients. Using recombinant technology, they were able to identify, sequence, and mass produce antibodies from B-cell clones from individual MS patients. Importantly, they have been able to identify a foreign antigen recognized by B-cell clones from an early primary progressive MS patient. Investigation of this common antigen as a possible autoimmune trigger in MS is ongoing. Jerry Lin is also working to establish appropriate risk assessment tools to predict the development of progressive multifocal leukoencephalopathy (PML) in natalizumab-treated MS patients through generating several tools to detect the presence of John Cunningham virus (JCV), the causative agent of PML. His extensive research reflects his enthusiasm and dedication to not only pursuing a cure for multiple sclerosis but to the Center itself.
Details

Kriti Kalpana, PhD joined the Tisch MSRCNY team as a Research Associate in early 2025. Previously, Kriti served as a Staff Scientist at the New York Stem Cell Foundation Research Institute, where she also performed postdoctoral research. Her work at NYSCF involved launching organoids, both from healthy individuals and those with MS and Parkinson’s Disease, into Low-Earth Orbit for a month-long study aboard the International Space Station. She completed her Biochemistry PhD at the Hunter College in New York City.
At Tisch MSRCNY, Kriti's research focuses on using organoid models to study the causes and disease progression of different subtypes of Multiple Sclerosis. Her work aims to examine phenotypic and functional differences across MS subtypes and leverage 3D neuro-immune assembloid cultures to explore the role of glial cells in MS and identify potential functional biomarkers of the disease.
Research Assistants
Since 2006, we have trained over 140 college graduates as research assistants (RAs) for 2-year rotations. While at Tisch, the RAs are all expected to publish their research and taught to critically review the literature at weekly conferences and laboratory meetings. After completing this rigorous program at Tisch MSRCNY, our RAs are almost always able to obtain placement in leading MD, PhD, or MD/PhD graduate programs.
To learn more, visit our Careers page.

Staff
Details

Talene Kelly oversees all of Tisch MS Research Center of New York’s fundraising initiatives, donor relations, and events. As Director of Development, Talene works closely with the Board of Directors and Executive Director to identify and build cases for support of Tisch MSRCNY’s research programs while developing and driving fundraising strategies.
Talene has spent over 10 years in development. Her additional experience includes co-founding the Taste of Battery Park City and raising funds for Pulmonary Fibrosis. Talene holds a BA in Creative Writing from The New School.
Details

Amanda Oppenheimer joined the Tisch MS Research Center in November 2014 as the organization’s Controller. Amanda graduated from the University of Arizona with a Bachelor of Science in Accounting and earned her CPA license in the spring of 2010. She has experience in accounting and auditing, as well as taxation. Before joining Tisch MSRCNY, Amanda worked in New York City at several regional, national and international public accounting firms. Amanda works closely with the Board of Directors and Dr. Sadiq to ensure proper financial controls are in place as we continue our mission to find the cause of and cure for multiple sclerosis. In the summer of 2016, she was promoted to Chief Financial Officer and in July of 2018, Amanda was promoted to Chief Operating Officer.
Details

Caitlin Smith is an enthusiastic Laboratory Operations Manager with experience working in both Academia and Industry. She earned her BSc in Human Genetics from University College London in 2011, and then went on to pursue her PhD in Molecular Biology from the Wilson Laboratory at Albert Einstein College of Medicine where she characterized the K15P protein of KSHV in primary effusion lymphoma cells (graduating in 2018). After graduating, she worked in the Jorge Reis-Filho laboratory at MSKCC elucidating the molecular mechanisms of rare tumors and managing the research laboratory.
Caitlin previously served as a Laboratory Operations Scientist and Lab Manager at several gene therapy start-ups, including Prevail therapeutics (now a wholly owned subsidiary of Elli Lilly) and Lexeo therapeutics, where she spearheaded the Lab build out and expansion, overseeing multiple research groups. Her experience includes EHS, permitting and compliance, equipment maintenance and calibration, inventory management, personnel training and development, budget administration and financial oversight, SOPs and Lab instruction development, QA collaboration and support, effective cross-functional teamwork and external stakeholder communication.
In her free time she enjoys listening to WFMU radio, going to see live music and biking everywhere.